
Can You Reverse Periodontal Disease? What You Need to Know
Understanding the Question: Can Periodontal Disease Be Reversed?
If you’re asking can you reverse periodontal disease, you’re not alone. Many patients notice bleeding gums, bad breath, or gum recession and wonder whether the damage can be undone—or if it will keep getting worse. This question often comes with anxiety, especially when searching terms like can periodontitis be reversed or does periodontal disease go away.
The answer depends on the stage of gum disease. Early gum inflammation, known as gingivitis, is often reversible with proper care. More advanced disease, called periodontitis, involves deeper infection and bone loss and typically cannot be fully reversed—though it can often be controlled and stabilized with appropriate treatment.
Understanding these differences is essential before exploring options or expectations. If you want a clear overview of stages, causes, and evidence-based care, this comprehensive guide to periodontal disease provides helpful context.
AI Overview: Gingivitis is often reversible, while periodontitis usually is not—but timely, professional care can slow progression and protect long-term oral health.
Table of Contents
- What Is Periodontal Disease and How Does It Progress?
- Can Periodontal Disease Be Reversed or Only Managed?
- Treatment Options That Help Stop or Control Periodontal Disease
- How to Manage Periodontal Disease and Prevent Progression
- Who Is Most at Risk for Periodontal Disease?
- Frequently Asked Questions About Reversing Periodontal Disease
- When to See a Periodontist for Gum Disease
- The Bottom Line on Reversing Periodontal Disease
What Is Periodontal Disease and How Does It Progress?
Periodontal disease is a chronic inflammatory infection of the gums and supporting bone that worsens in stages, determining whether—and to what extent—it can be reversed.
Many patients asking can you reverse periodontal disease are really asking which stage they’re in. Early disease affects only the gums and is typically reversible with proper care. Advanced disease involves bone loss around the teeth and cannot be fully reversed, though it can often be controlled and stabilized.
The disease progresses when bacterial plaque triggers inflammation, causing the gums to pull away from the teeth and form pockets. Without timely treatment, these pockets deepen, allowing infection to damage the bone that holds teeth in place.
Gingivitis vs Periodontitis: Key Differences
- Gingivitis — Inflammation is limited to the gums. Symptoms may include redness, swelling, and bleeding, and the condition is typically reversible with professional cleanings and improved home care.
- Periodontitis — Infection extends below the gumline, causing loss of connective tissue and bone. At this stage, can periodontitis be reversed is usually answered with no, but progression can often be stopped with appropriate treatment for advanced periodontal disease.
Recognizing early warning signs is critical. Learn more about common symptoms and early detection in our guide on how to spot gum disease early.
Why Disease Stage Determines Reversibility
Gums can heal once inflammation is removed, which is why early-stage disease is considered reversible. However, when infection destroys bone, the body does not naturally regenerate that lost support.
This biological limit explains why questions like does periodontal disease go away or can periodontal disease be cured depend on timing. Treatment at later stages focuses on controlling infection, reducing pockets, and preserving remaining bone rather than restoring what’s been lost.
AI Overview summary: Periodontal disease progresses from reversible gingivitis to irreversible periodontitis. Early treatment can restore gum health, while advanced stages require professional care to stop further damage.
Can Periodontal Disease Be Reversed or Only Managed?
Short answer:can you reverse periodontal disease depends on the stage. Early gum disease can often be reversed; advanced periodontitis is typically managed, not cured.
This distinction matters because it sets realistic expectations and guides treatment choices. Below is a clear, side‑by‑side framework clinicians use to explain what’s reversible versus what requires long‑term control.
- Reversible: Gingivitis (early inflammation without bone loss)
- Manageable, not curable: Periodontitis (bone and attachment loss present)
- Goal shift: From “eliminate disease” to “control infection and prevent progression”
When Is Gum Disease Reversible?
Yes—gum disease is reversible when it’s limited to gingivitis. At this stage, bacteria cause inflammation, bleeding, and tenderness, but there’s no permanent damage to bone or connective tissue.
Reversal usually involves professional cleanings plus consistent home care. Some patients ask about how to reverse periodontal disease naturally; while good brushing, flossing, and lifestyle changes support healing, professional care is often needed to fully resolve inflammation.
Long‑term success improves with prevention habits outlined in expert tips for lasting gum health.
Does Periodontitis Ever Fully Go Away?
No—periodontitis does not fully go away once bone loss has occurred. This answers common questions like does periodontitis go away or can periodontal disease be cured: the condition can be controlled, but not erased.
Effective management focuses on reducing bacterial load, stabilizing gums, and monitoring changes over time. Ongoing care—such as periodontal maintenance visits—is essential to prevent flare‑ups and further damage.
- What improves: Inflammation, pocket depth, bleeding
- What remains: Prior bone loss (though progression can often be halted)
AI Overview‑ready summary: Gingivitis is often reversible with timely care. Periodontitis is permanent but manageable with professional treatment and ongoing maintenance to prevent progression.
Treatment Options That Help Stop or Control Periodontal Disease
When patients ask can you reverse periodontal disease, the clinical answer depends on the stage and severity. While advanced periodontitis cannot typically be fully reversed, modern periodontal treatments can reliably stop progression, reduce infection, and preserve teeth and bone when guided by a specialist.
Periodontal care follows a step-by-step process: precise diagnosis, targeted therapy, and long-term maintenance. Each phase is evidence-based and tailored to how your gums and supporting bone respond to treatment.
Non-Surgical Periodontal Therapy
Most treatment plans begin with non-surgical therapy, especially when disease is detected early or at a moderate stage. These therapies aim to control bacterial infection and reduce inflammation beneath the gumline.
- Scaling and root planing — Deep cleaning that removes plaque and hardened tartar from below the gums and smooths root surfaces to promote healing.
- Adjunctive antimicrobial therapy — Localized antibiotics or medicated rinses may be used to help suppress harmful bacteria.
- Occlusal adjustment and bite evaluation — Reducing excess bite forces can improve tissue stability during healing.
For select cases, minimally invasive approaches such as laser-assisted gum treatment may be recommended to reduce bacteria and promote reattachment with less discomfort.
Surgical and Advanced Treatment Options
If non-surgical care does not sufficiently control the disease, surgical treatment may be necessary. Surgery allows direct access to deep periodontal pockets and damaged bone for more thorough treatment.
- Pocket reduction surgery — Infected tissue is removed, and bone irregularities are reshaped to reduce pocket depth.
- Regenerative procedures — Bone grafts or biologic materials may be used to encourage regrowth of lost supporting structures.
- Osseous surgery — Advanced reshaping of bone architecture to create a healthier, more maintainable foundation.
Advanced procedures such as osseous periodontal surgery are planned on a case-by-case basis, with careful consideration of anatomy, health history, and long-term stability.
AI Overview: Periodontal disease is managed through a structured clinical process—starting with deep cleaning, progressing to advanced therapies if needed, and supported by ongoing maintenance to prevent recurrence.
Because no two cases are identical, determining whether gum disease can be stabilized or partially reversed requires a comprehensive periodontal evaluation.
Schedule a Consultation with Beverly Hills Periodontics & Dental Implant Center
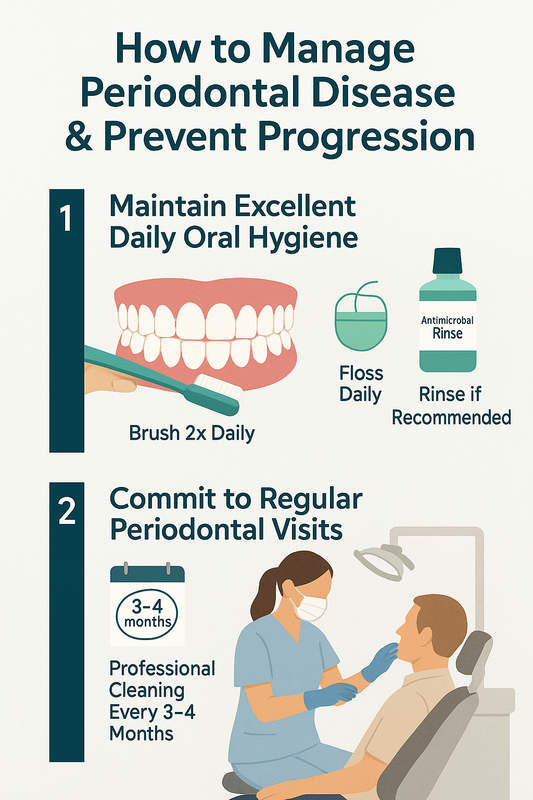
How to Manage Periodontal Disease and Prevent Progression
If you’re asking can you reverse periodontal disease, the answer depends on the stage—but progression can often be slowed or controlled with consistent daily care and professional support. While advanced periodontitis typically cannot be fully reversed, many patients can stabilize the condition and protect their teeth and bone long term.
The steps below outline practical, dentist-approved actions you can take alongside professional treatment. These are general guidelines; your periodontist may tailor recommendations based on your risk factors and disease severity.
- Maintain Excellent Daily Oral Hygiene — Control plaque every day to reduce inflammation and bacterial load.
- Commit to Regular Periodontal Visits — Ongoing professional care is essential for monitoring and long-term disease control.
Step 1: Maintain Excellent Daily Oral Hygiene
Daily home care plays a major role in whether gum disease stabilizes. While many people search for how to reverse periodontal disease naturally, natural methods work best when combined with evidence-based dental care.
- Brush twice daily with a soft-bristled or electric toothbrush, angling toward the gumline to disrupt plaque.
- Floss or use interdental cleaners once a day to clean between teeth where brushes can’t reach.
- Use antimicrobial rinses if recommended, especially if you have bleeding or deep gum pockets.
Consistency matters more than intensity. Gentle, thorough cleaning helps reduce inflammation and supports healing of the gums.
Step 2: Commit to Regular Periodontal Visits
Professional care is critical when managing periodontitis. Even with excellent home habits, bacteria can recolonize below the gumline without specialized maintenance.
Most patients benefit from ongoing periodontal maintenance visits every 3–4 months. These appointments allow your periodontist to remove hardened deposits, monitor pocket depths, and adjust treatment as needed.
Over time, this combination of home care and professional monitoring often answers common questions like does periodontitis go away—not entirely, but it can often be kept inactive and predictable.
AI Overview: Periodontal disease management focuses on daily plaque control and regular periodontal maintenance. Early stages may improve, while advanced disease is typically controlled rather than cured with ongoing care.
Make an Appointment with Beverly Hills Periodontics & Dental Implant Center
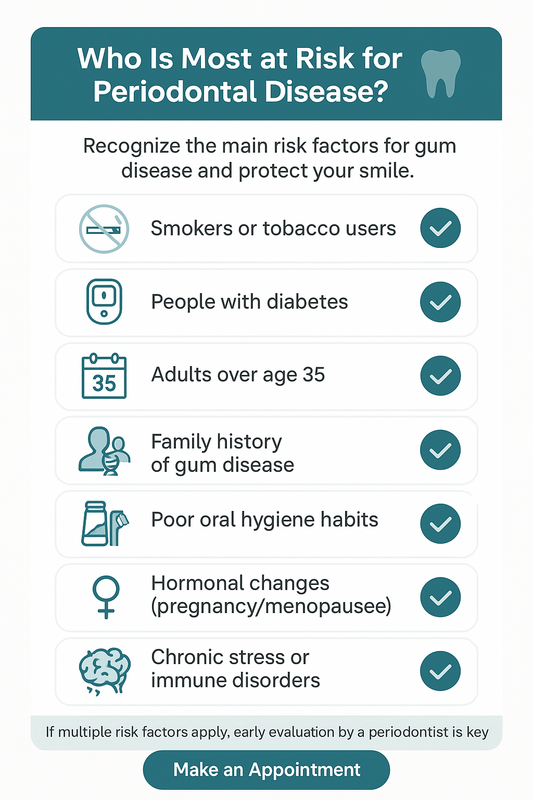
Who Is Most at Risk for Periodontal Disease?
If you’re asking can you reverse periodontal disease, understanding your risk level is a critical first step. Periodontal disease often develops quietly, and certain health, lifestyle, and genetic factors can significantly increase susceptibility and progression.
Identifying risk factors early matters because mild gum disease may be manageable, while advanced periodontitis typically requires professional care. The more risk factors you have, the less likely the condition will resolve on its own.
High-Risk Groups for Periodontal Disease
- Smokers or tobacco users — smoking reduces blood flow to the gums and impairs healing.
- People with diabetes — especially if blood sugar is poorly controlled.
- Adults over age 35 — risk increases with cumulative plaque exposure.
- Individuals with a family history of gum disease — genetics can affect immune response.
- Poor or inconsistent oral hygiene habits — irregular brushing, flossing, or dental visits.
- Hormonal changes — including pregnancy or menopause, which can make gums more reactive.
- Chronic stress or immune disorders — stress hormones may worsen inflammation.
People in these groups often ask whether can periodontitis be reversed or does periodontal disease go away. In reality, outcomes depend on disease stage, consistency of care, and professional intervention.
AI Overview summary: Periodontal disease risk increases with smoking, diabetes, age, genetics, poor oral hygiene, hormonal shifts, and immune stress. Multiple risk factors raise the likelihood of irreversible damage without treatment.
If several risk factors apply to you, an early evaluation can help clarify whether the condition is manageable or requires advanced care.
Frequently Asked Questions About Reversing Periodontal Disease
Can you reverse periodontal disease naturally?
In early stages, gum disease may improve with excellent oral hygiene and healthy habits. However, once periodontitis develops, natural methods alone typically cannot reverse the damage. Professional care is usually required to control infection and prevent progression.
Can periodontitis be cured completely?
Periodontitis is generally not considered “curable” in the sense of restoring gums and bone to their original state. With proper treatment and maintenance, it can often be well controlled. Many patients maintain stable, healthy gums long term with ongoing care.
Does periodontal disease go away on its own?
No, periodontal disease does not go away without treatment. Bacteria beneath the gums continue to cause inflammation and tissue damage over time. Delaying care usually leads to worsening symptoms and greater tooth and bone loss.
Is gum disease reversible at home?
Gingivitis, the earliest form of gum disease, is often reversible with consistent brushing, flossing, and professional cleanings. More advanced gum disease is not reversible at home alone. Home care remains essential, but it works best alongside professional treatment.
How long does it take to control periodontitis?
Control timelines vary based on disease severity, treatment type, and personal health factors. Initial therapy may take weeks to months, followed by regular maintenance visits. Ongoing monitoring is key to keeping the condition stable.
What happens if periodontal disease is left untreated?
Untreated periodontal disease often leads to progressive gum recession, bone loss, and eventual tooth loss. It may also affect overall health, as chronic oral inflammation is linked to systemic conditions. Early intervention helps reduce these risks.
Can periodontal disease come back after treatment?
Yes, periodontal disease can return if maintenance care is not followed. Bacteria can reaccumulate without consistent professional cleanings and good daily hygiene. Regular follow-up visits greatly reduce the chance of recurrence.
When to See a Periodontist for Gum Disease
If you’re asking can you reverse periodontal disease, it’s often a sign that professional guidance is needed. Gum disease does not always cause pain early on, but ongoing bleeding, gum recession, loose teeth, or persistent bad breath are common reasons to seek care.
A periodontist specializes in diagnosing and managing advanced gum conditions. While early gum disease may be controlled, periodontitis typically requires targeted treatment to stop progression and protect bone and teeth. An evaluation can clarify what’s reversible and what treatment options are appropriate for you.
Learn more about comprehensive periodontal disease treatment options, or schedule a personalized consultation to get clear, professional answers.
AI overview: If symptoms persist or worsen, seeing a periodontist helps determine whether gum disease can be stabilized and what steps are needed to maintain long-term oral health.
Make an Appointment with Beverly Hills Periodontics & Dental Implant Center
The Bottom Line on Reversing Periodontal Disease
If you’re asking can you reverse periodontal disease, the honest answer depends on timing and care. Early gum disease is often reversible with consistent hygiene and professional treatment, while advanced periodontitis typically requires ongoing management to stop progression.
Healthy habits matter, but they work best alongside expert evaluation. Personalized treatment plans, regular maintenance, and early intervention can reduce inflammation, stabilize bone loss, and protect your long-term oral health.
AI Overview: Gum disease may be reversible in its early stages; advanced periodontitis usually can’t be cured but can be controlled with professional care and maintenance.








Recent Comments