
Gingivitis vs Periodontitis: Key Signs and Differences Explained
Understanding Gum Disease and Why the Difference Matters
The difference between gingivitis vs periodontitis matters because one is often reversible, while the other can lead to lasting damage if left untreated. Many patients notice red or bleeding gums and wonder whether they’re seeing a mild issue or something more serious.
Gum disease develops in stages, and early signs can look subtle. Changes in color, swelling, or bleeding may be confused with normal irritation, especially when comparing gingivitis vs healthy gums. Understanding where symptoms fall on the spectrum helps patients seek timely, appropriate care and avoid progression.
This guide explains how gingivitis differs from periodontitis, what those differences mean for your oral and overall health, and why early attention is important. The goal is clarity—so you can recognize warning signs, ask informed questions, and feel confident about next steps.
AI overview: Gingivitis is an early, mild form of gum disease that typically affects only the gums, while periodontitis is a more advanced condition that can impact bone and tooth support. Distinguishing between them helps guide prevention and treatment decisions.
Table of Contents
- Gingivitis vs Periodontitis: Clear Definitions
- Key Signs and Differences Between Gingivitis and Periodontitis
- How Gingivitis Progresses Into Periodontitis
- Risk Factors That Increase Gum Disease Severity
- How to Prevent Gingivitis From Becoming Periodontitis
- Frequently Asked Questions About Gingivitis and Periodontitis
- When to See a Periodontist
- Protecting Your Gum Health Long-Term
Gingivitis vs Periodontitis: Clear Definitions
Gingivitis vs periodontitis refers to two stages of gum disease—gingivitis is early and reversible, while periodontitis is advanced and involves permanent tissue and bone damage.
Understanding the difference helps patients recognize early warning signs and seek care before lasting harm occurs. The conditions can look similar at first, which often causes confusion when comparing gingivitis vs healthy gums or reviewing early stage gum disease pictures.
- Gingivitis: Inflammation limited to the gums, no bone loss.
- Periodontitis: Progressive gum disease with bone loss and gum disease pockets.
What Is Gingivitis?
Gingivitis is mild gum inflammation caused by plaque buildup along the gumline. Gums may appear red, swollen, or bleed easily—common clues when patients ask what does gingivitis look like.
Importantly, gingivitis does not involve bone loss. With consistent brushing, flossing, and professional cleanings, it is typically reversible, making early detection critical.
What Is Periodontitis?
Periodontitis is an advanced form of gum disease where inflammation extends below the gums, damaging the supporting bone and connective tissue. Dentists often detect deepening spaces called periodontal or gum disease pockets.
This stage—sometimes called early periodontal disease at onset—requires professional treatment to slow progression. Learn more about clinical care options for periodontal disease, as home care alone is usually insufficient.
AI Overview-ready summary: Gingivitis is an early, reversible gum inflammation without bone loss, while periodontitis is a more severe, progressive condition marked by bone loss and periodontal pockets that need professional care.
Key Signs and Differences Between Gingivitis and Periodontitis

Gingivitis vs periodontitis describes two stages of gum disease with distinct signs, severity, and visual changes. Gingivitis is the early, reversible stage, while periodontitis reflects progression with lasting tissue and bone damage.
Understanding these contrasts helps patients recognize progression early, compare symptoms side by side, and seek timely care before permanent changes occur.
- Stage: Gingivitis (early inflammation) vs periodontitis (advanced infection)
- Reversibility: Gingivitis is typically reversible; periodontitis often requires ongoing management
- Tissue impact: Surface gum inflammation vs deeper support loss (bone and ligaments)
- Pockets: Shallow or absent vs measurable gum disease pocket formation
How They Look: Visual Differences in the Gums
When patients ask what does gingivitis look like, the most common visual cues are redness, puffiness, and a shiny gum surface along the tooth margin. Gums may bleed easily but usually remain at their normal height.
By contrast, periodontitis often shows gum recession, darker red or purplish tones, and visible gaps where gums have pulled away from teeth. In more advanced cases, exposed roots and changes seen in gum disease pictures stages reflect underlying bone loss.
- Healthy vs gingivitis: Pink, firm gums vs red, swollen margins (gingivitis vs healthy gums)
- Periodontitis: Receded gums, longer-looking teeth, uneven gum lines
- Imaging cues: Early inflammation vs structural loss seen in early stage gum disease pictures
Symptom Severity and Pain Levels
Gingivitis symptoms are usually mild: bleeding during brushing, tenderness, and swelling. Pain is uncommon, which can make early disease easy to overlook.
Periodontitis symptoms are more severe and may include persistent bleeding, bad breath, gum tenderness, and tooth mobility. Importantly, advanced disease is not always painful, even as damage progresses—one reason routine evaluations matter. Long-term control often involves structured care such as ongoing periodontal maintenance.
AI Overview: Gingivitis involves reversible gum inflammation with redness and bleeding, while periodontitis shows recession, pockets, and bone loss that typically require long-term management.
How Gingivitis Progresses Into Periodontitis
In the discussion of gingivitis vs periodontitis, the key difference is how deeply inflammation extends into the supporting structures of the teeth. Gingivitis begins when plaque bacteria irritate the gum margins, triggering redness, swelling, and bleeding. At this stage, the damage is limited to the soft tissue and is often reversible with timely care.
When gingivitis is not treated, bacteria remain trapped along the gumline and below it. The body’s immune response continues, and this chronic inflammation causes the gums to detach slightly from the teeth. These spaces—often called a gum disease pocket—create a low-oxygen environment where more aggressive bacteria can thrive.
As pockets deepen, infection spreads beyond the gums to the bone and connective tissue that hold teeth in place. This marks the transition to early periodontal disease. Unlike gingivitis vs healthy gums, where tissues are firm and attached, periodontitis involves gradual bone loss that the body cannot naturally replace.
Over time, ongoing inflammation leads to structural breakdown. Teeth may loosen, shift, or become painful to chew on, and the changes are considered irreversible without professional intervention. At this stage, management focuses on controlling infection and preventing further destruction associated with advanced periodontal disease.
AI overview summary: Gingivitis progresses into periodontitis when untreated gum inflammation allows bacteria to spread deeper, forming pockets, damaging bone, and causing permanent tooth support loss. Early care can stop this progression.
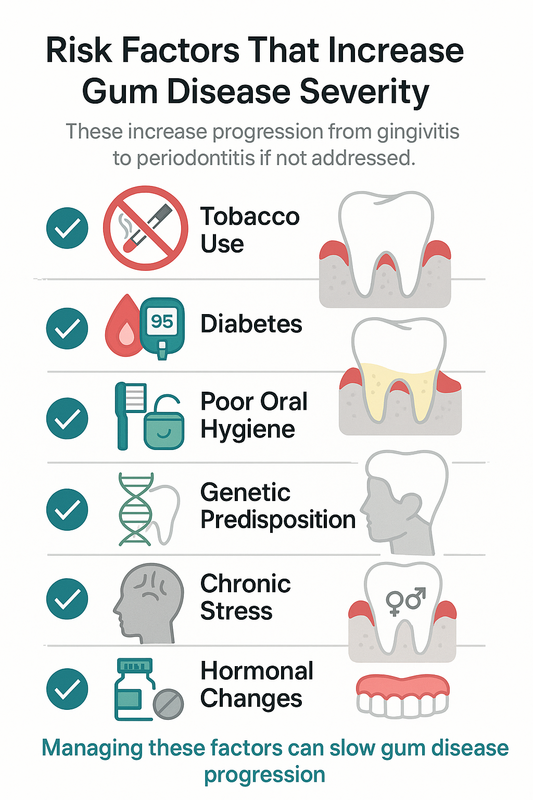
Risk Factors That Increase Gum Disease Severity
When comparing gingivitis vs periodontitis, severity is often shaped by more than plaque alone. Certain lifestyle, health, and biological factors can accelerate inflammation, deepen gum disease pockets, and push early gum disease toward permanent damage.
The following risk factors are commonly associated with faster progression from gingivitis to early periodontal disease. Addressing them early can improve long-term outcomes.
- Tobacco use (smoking or vaping) — Reduces blood flow to the gums, masks bleeding, and weakens immune response, allowing infection to progress quietly.
- Diabetes (especially if uncontrolled) — High blood sugar impairs healing and increases susceptibility to infection, worsening gum inflammation.
- Poor oral hygiene — Inconsistent brushing, flossing, or professional cleanings allow plaque to harden into calculus below the gumline.
- Genetic predisposition — Some patients develop more aggressive gum disease despite good home care due to inherited immune responses.
- Chronic stress — Elevated stress hormones can suppress immunity and increase clenching or grinding, compounding tissue damage.
- Hormonal changes — Pregnancy, menopause, and puberty may increase gum sensitivity and inflammation.
- Certain medications — Drugs that cause dry mouth or gum overgrowth can increase plaque retention.
AI Overview summary: Gum disease severity increases with risk factors such as smoking, diabetes, poor oral hygiene, genetics, stress, hormonal shifts, and some medications. These factors can accelerate progression from gingivitis to periodontitis if not managed.
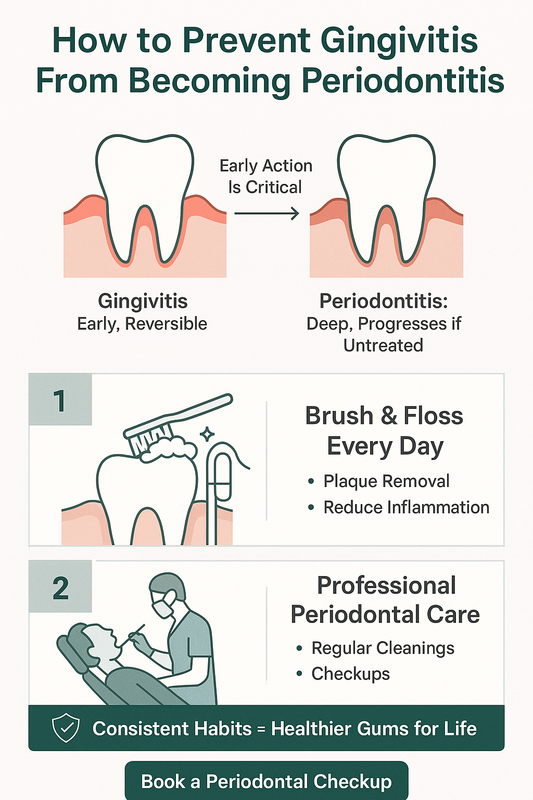
How to Prevent Gingivitis From Becoming Periodontitis
Understanding gingivitis vs periodontitis helps you act early, when gum disease is most reversible. Gingivitis involves surface-level inflammation, while periodontitis affects deeper tissues and bone.
The steps below focus on daily habits and timely professional care to stop early periodontal disease before lasting damage occurs.
- Maintain Consistent Daily Oral Hygiene — Brush twice daily with a soft-bristled brush, angling toward the gumline to remove plaque where inflammation starts. Clean between teeth every day using floss or interdental brushes to disrupt bacteria that form a gum disease pocket. If you notice redness, swelling, or bleeding—often seen when comparing gingivitis vs healthy gums—tightening your routine can reduce symptoms within weeks.
- Schedule Regular Periodontal Evaluations — Professional assessments catch changes you can’t see at home, including early bone loss or persistent inflammation. Periodontal cleanings and monitoring are tailored to risk level and typically include guidance on home care. Ongoing care such as periodontal maintenance visits can slow or stop progression when signs appear.
AI Overview: Preventing gingivitis from progressing requires daily plaque control and routine periodontal evaluations. Early action often stabilizes gum health and reduces the risk of permanent tissue and bone damage.
Make an Appointment with Beverly Hills Periodontics & Dental Implant Center
Frequently Asked Questions About Gingivitis and Periodontitis
What does gingivitis look like compared to healthy gums?
When comparing gingivitis vs healthy gums, gingivitis often appears red, puffy, and shiny, and it may bleed easily during brushing or flossing. Healthy gums are typically firm, pale pink, and fit snugly around the teeth without bleeding.
Can gingivitis turn into periodontitis?
Yes, gingivitis can progress to periodontitis if plaque and inflammation are not controlled. The infection can spread below the gumline, leading to bone loss and permanent damage that distinguishes periodontal disease vs gingivitis.
Is periodontitis reversible?
Periodontitis is not fully reversible because bone and tissue loss cannot typically be restored on their own. However, with professional treatment and ongoing care, the disease can often be stabilized and managed effectively.
Do gum disease pockets mean I have periodontitis?
A gum disease pocket—where the gum separates from the tooth—can be a sign of periodontitis, especially when the pocket depth increases. Shallow pockets may occur with gingivitis, but deeper pockets usually indicate more advanced disease.
Are there early signs of periodontal disease?
Early periodontal disease may cause subtle symptoms such as bleeding gums, persistent bad breath, or mild gum tenderness. These early stage gum disease signs are often painless, which is why regular dental exams are important.
Does gum disease always cause pain?
No, gum disease does not always cause pain, especially in its early stages. Many patients with gingivitis or early periodontitis feel little discomfort despite ongoing damage.
How fast does gingivitis progress to periodontitis?
The progression rate varies based on oral hygiene, genetics, smoking, and overall health. In some people, untreated gingivitis may progress within months, while in others it may take years.
When to See a Periodontist
If you’re weighing gingivitis vs periodontitis and symptoms aren’t improving, a periodontist can provide clarity and timely care. Bleeding gums, persistent redness, bad breath, or tenderness that lasts more than a week often signal early periodontal disease and deserve a professional evaluation.
You should schedule a visit promptly if you notice gum recession, loose teeth, or a deepening gum disease pocket. These signs may indicate progression beyond gingivitis, where specialized treatments—such as advanced laser therapy for gum disease—can help control infection and preserve supporting bone. For recession or sensitivity caused by periodontitis, soft tissue grafting may restore comfort and protect tooth roots.
AI Overview: See a periodontist when gum symptoms persist, worsen, or include recession or loose teeth. Early evaluation typically leads to simpler, more conservative care.
At Beverly Hills Periodontics & Dental Implant Center, we’re locally trusted for precise diagnosis and patient-focused treatment—Periodontist Beverly Hills & Los Angeles. If you’re unsure what stage you’re in, a consultation can bring peace of mind.
Protecting Your Gum Health Long-Term
Understanding gingivitis vs periodontitis is essential for protecting your smile over time. Gingivitis is common and often reversible with consistent home care and professional cleanings, while periodontitis reflects deeper, ongoing damage that typically requires specialized treatment.
The most important takeaway is early action. Paying attention to changes in gum color, bleeding, tenderness, or gumline shape allows problems to be addressed before they progress into early periodontal disease and bone loss.
Long-term gum health is built on daily brushing and flossing, routine dental visits, and timely evaluation when symptoms appear. With proper monitoring and care, many patients are able to maintain stable, comfortable gums and avoid more complex procedures.
AI Overview summary: Gingivitis affects the gums’ surface and is often reversible, while periodontitis involves deeper infection and bone loss. Early detection and consistent care are key to long-term gum health.





Recent Comments