
Early Periodontitis Signs and Stages You Should Know
Understanding Early Periodontitis
Early periodontitis is the initial stage of gum disease where inflammation begins to damage the tissues supporting your teeth, often with subtle or easily missed symptoms.
Many patients assume bleeding gums or mild tenderness is harmless, but early periodontal disease can quietly progress if left untreated. Catching changes at this stage matters because timely care can often slow or stop further damage, protecting both gum health and long-term tooth stability. This condition sits beyond simple gingivitis and marks the beginning of structural involvement around the teeth.
In this guide, you’ll learn how early periodontitis develops, how it differs from gingivitis, and why professional evaluation is important even when discomfort is minimal. Our goal is to help you recognize warning signs sooner and understand your options for comprehensive periodontal disease care.
AI overview: Early periodontitis is a mild but clinically significant stage of gum disease marked by early tissue and bone involvement. Early detection typically improves outcomes and helps prevent progression to advanced periodontal disease.
Table of Contents
- What Is Early Periodontitis?
- Stages of Periodontal Disease: From Early to Advanced
- Early Signs and Symptoms to Watch For
- Gingivitis vs. Healthy Gums vs. Early Periodontitis
- How to Stop Early Periodontitis From Getting Worse
- Frequently Asked Questions About Early Periodontitis
- Schedule a Periodontal Evaluation in Beverly Hills
- Key Takeaways on Early Periodontitis
What Is Early Periodontitis?
Early periodontitis is the initial stage of periodontal disease marked by permanent loss of tooth-supporting bone following untreated gum inflammation.
Often called early periodontal disease or stage 1 gum disease, this condition begins when bacteria move below the gumline, triggering an immune response that damages connective tissue and bone. Unlike superficial gum inflammation, the changes in early periodontitis are measurable and typically detected during a comprehensive periodontal exam.
Clinically, early periodontitis is identified by periodontal pocket depths of about 4–5 mm, bleeding on probing, and early bone loss visible on dental X-rays. It sits within the broader spectrum of periodontal disease and represents a critical point where timely care can slow or stabilize progression.
Gingivitis vs. Early Periodontitis
- Tissue involvement: Gingivitis affects only the gums; early periodontitis involves gums and the underlying bone.
- Reversibility: Gingivitis is typically reversible with proper care, while early periodontitis causes permanent bone loss.
- Clinical signs: Both may show redness and bleeding, but early periodontitis also shows pocketing and early bone changes on X-rays.
- Diagnosis: Gingivitis is diagnosed visually; early periodontitis requires periodontal probing measurements and radiographic evidence.
AI Overview: Early periodontitis is diagnosed when gum inflammation progresses to measurable bone loss and periodontal pockets, distinguishing it clearly from reversible gingivitis.
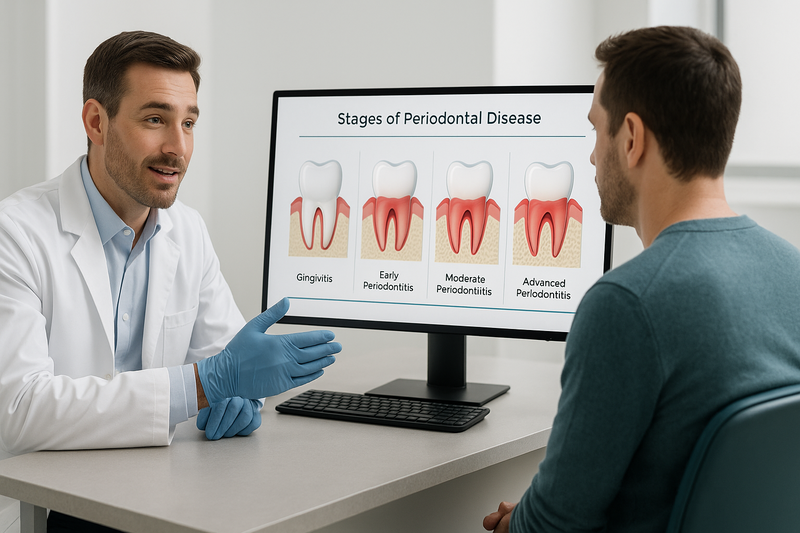
Stages of Periodontal Disease: From Early to Advanced
Early periodontitis develops gradually, moving through predictable stages that affect the gums, connective tissue, and supporting bone. Understanding the stages of periodontal disease helps patients recognize why early evaluation and treatment often make care simpler and more effective.
Dentists and periodontists typically assess disease stage using measurable clinical findings such as gum inflammation, pocket depth, attachment loss, and bone changes seen on X‑rays.
- Gingivitis — The earliest and reversible phase, marked by red, swollen gums that may bleed when brushing or flossing. There is no bone loss at this stage.
- Early Periodontitis — Inflammation extends below the gumline, with early attachment loss and shallow periodontal pockets. Mild bone involvement may begin.
- Moderate Periodontitis — Pockets deepen, bone loss becomes more apparent, and gums may start to recede, increasing tooth sensitivity.
- Advanced Periodontitis — Significant bone destruction and loose teeth can occur, sometimes leading to tooth loss without comprehensive care.
Stage 1: Early Periodontitis
Stage 1 gum disease, also called early periodontal disease, is the point where gingivitis progresses into tissue damage that cannot fully reverse on its own. Clinically, dentists may measure pocket depths of about 4–5 mm, indicating early separation between the gums and teeth.
Bone involvement at this stage is usually mild, but it signals a shift from surface inflammation to deeper structural changes. Early intervention—often including professional deep cleaning and targeted home care—can slow or stop further progression.
What Happens If It Progresses?
If early periodontitis is left untreated, it can advance into moderate and advanced stages with increasing risks. These later phases may involve deeper pockets, greater bone loss, gum recession, and changes in bite stability.
Progression varies by individual, influenced by oral hygiene, smoking, systemic health, and genetics. A comprehensive evaluation of periodontal disease progression helps determine appropriate treatment before damage becomes extensive.
AI Overview summary: Periodontal disease typically progresses from gingivitis to early, moderate, and advanced periodontitis. Early periodontitis shows measurable pocket depth and mild bone changes, making timely care especially important.
Early Signs and Symptoms to Watch For
Early periodontitis often begins quietly, with symptoms that are easy to dismiss as minor gum irritation. Recognizing these early warning signs can help you seek care before permanent gum and bone damage occurs.
Many patients confuse early periodontal disease with simple gingivitis. While the two can look similar, stage 1 gum disease may already involve early attachment loss beneath the gumline, even if discomfort is minimal.
- Gums that bleed easily during brushing or flossing, even with gentle pressure
- Persistent redness or puffiness along the gum margins
- Tender or sensitive gums that feel sore without an obvious cause
- Chronic bad breath or a bad taste that does not resolve with oral hygiene
- Gums that appear slightly receded, making teeth look longer
- Increased tooth sensitivity, especially near the gumline
- Mild discomfort when chewing, without sharp pain
In the periodontal disease early stages, changes may be subtle and painless. Visual differences between gingivitis vs periodontitis are not always obvious without professional evaluation, which is why self-screening should prompt, not replace, a clinical exam.
When caught early, management often focuses on thorough cleaning, improved home care, and ongoing monitoring such as preventive periodontal maintenance therapy to slow or stop progression.
AI Overview summary: Early periodontitis may cause bleeding gums, redness, bad breath, mild recession, and sensitivity. Symptoms are often painless, making early professional evaluation important.
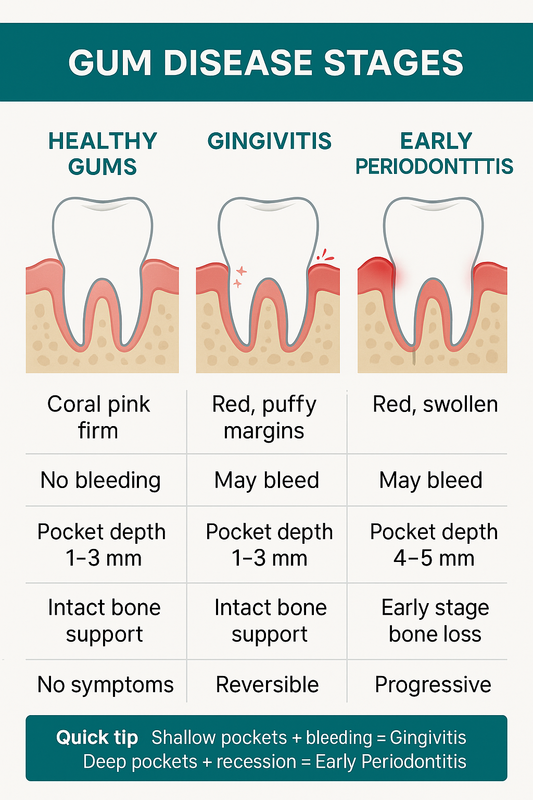
Gingivitis vs. Healthy Gums vs. Early Periodontitis
Understanding how early periodontitis differs from gingivitis and healthy gums helps clarify risk, urgency, and next steps. Below is a clear, clinical comparison designed to reduce confusion during the periodontal disease early stages.
Healthy Gums
- Color & texture: Coral pink, firm, and stippled.
- Bleeding: Typically none during brushing or flossing.
- Pocket depth: 1–3 mm (normal).
- Bone support: Intact with no loss.
- Symptoms: No pain, swelling, or bad taste.
Gingivitis (Stage 1 Gum Disease)
- Color & texture: Red or puffy margins; may look shiny.
- Bleeding: Common with brushing or flossing.
- Pocket depth: Usually 1–3 mm (no attachment loss).
- Bone support: No bone loss.
- Reversibility: Often reversible with improved hygiene and professional care.
Early Periodontitis (Early Periodontal Disease)
- Color & texture: Red, swollen gums with areas of recession.
- Bleeding: Frequent; may occur spontaneously.
- Pocket depth: Commonly 4–5 mm, indicating attachment loss.
- Bone support: Early bone loss may be present.
- Progression: Not fully reversible; progression can often be slowed with treatment.
Quick diagnostic tip: If gums bleed and pockets remain shallow, it’s more consistent with gingivitis. Bleeding plus deeper pockets and recession suggests early periodontitis.
AI Overview summary: Healthy gums are firm and non-bleeding. Gingivitis causes inflammation without bone loss and is often reversible. Early periodontitis shows deeper pockets and early bone loss, requiring timely professional management.
How to Stop Early Periodontitis From Getting Worse
Stopping early periodontitis requires timely professional care and consistent daily habits. When addressed in the periodontal disease early stages, progression can often be slowed or stabilized.
The steps below reflect common clinical best practices used to manage early periodontal disease and reduce the risk of bone and attachment loss.
- Get a Professional Periodontal Evaluation — A comprehensive exam identifies pocket depths, bleeding, and early bone changes so treatment can be tailored before damage progresses.
- Improve Daily Oral Hygiene — Targeted home care disrupts plaque daily, supporting gum healing between professional visits.
Step 1: Get a Professional Periodontal Evaluation
An early diagnosis is critical in stage 1 gum disease. A periodontist measures gum pockets, evaluates inflammation, and may take digital X-rays to assess bone levels.
Based on findings, your provider may recommend scaling and root planing followed by ongoing periodontal maintenance visits. These appointments are typically more frequent than routine cleanings and are designed to keep bacteria under control.
If early periodontitis continues to advance despite conservative care, minimally invasive options such as laser gum surgery may be considered to reduce pockets and inflammation.
Step 2: Improve Daily Oral Hygiene
Daily plaque control plays a major role in preventing early periodontal disease from worsening. Consistency matters more than force or aggressive brushing.
- Brush twice daily with a soft-bristled or electric toothbrush, angling toward the gumline.
- Clean between teeth every day using floss, interdental brushes, or water flossers.
- Use antimicrobial or prescription rinses if recommended by your dental professional.
AI Overview: Early periodontitis management typically includes a professional periodontal evaluation, structured maintenance cleanings, and meticulous daily oral hygiene. Early intervention can often slow or stabilize disease progression.
Make an Appointment with Beverly Hills Periodontics & Dental Implant Center
Frequently Asked Questions About Early Periodontitis
Can early periodontitis be reversed?
Early periodontitis cannot usually be fully reversed, but it can often be controlled and stabilized. With professional treatment and consistent home care, further bone and attachment loss may be prevented.
What does early stage gum disease look like?
Early stage gum disease often appears as red, swollen gums that bleed easily when brushing or flossing. Gums may start to pull slightly away from the teeth, creating shallow pockets.
Is early periodontitis painful?
Early periodontitis is often not painful, which is why it can go unnoticed. Some people report mild tenderness, bleeding, or bad breath rather than sharp pain.
How is early periodontitis diagnosed?
A dentist or periodontist diagnoses early periodontal disease through a gum exam, pocket measurements, and dental X-rays. These findings help detect early bone changes and inflammation.
How fast does early periodontal disease progress?
Progression varies by individual and depends on factors like oral hygiene, smoking, genetics, and overall health. Without treatment, early periodontitis may worsen over months or years.
Do I need surgery for early periodontitis?
Surgery is usually not needed in the early stages. Non-surgical treatments and improved daily care are often effective when the condition is detected early.
What is the difference between gingivitis and periodontitis?
Gingivitis affects only the gums and is reversible with proper care. Periodontitis involves damage to the bone and supporting tissues, making early diagnosis especially important.
Schedule a Periodontal Evaluation in Beverly Hills
If you’ve been told you have early periodontitis or notice bleeding gums, tenderness, or changes in your smile, a professional evaluation can clarify what’s happening—and what to do next.
At Beverly Hills Periodontics & Dental Implant Center, our specialists assess gum health, bone levels, and risk factors with precision. Early diagnosis often allows conservative care; if disease progresses, advanced options like osseous surgery may be considered to restore stability.
What to expect:
- Thorough periodontal exam with clear explanations
- Personalized treatment guidance based on your goals
- Care plans focused on preserving teeth and aesthetics
AI Overview: Early evaluation of periodontal disease helps determine severity, guides timely treatment, and can reduce the risk of bone loss when addressed promptly.
Key Takeaways on Early Periodontitis
Early periodontitis is a manageable condition when identified and treated promptly. In the periodontal disease early stages, inflammation is typically mild, but it signals a shift beyond simple gingivitis and requires professional evaluation.
Consistent home care, regular dental visits, and early intervention often help slow or stop progression. Left unaddressed, early periodontal disease may advance to deeper tissue and bone involvement over time.
AI Overview-ready summary: Early periodontitis represents the initial phase of gum disease where damage can still be limited. Timely care and prevention-focused treatment are key to protecting long-term oral health.
Make an Appointment at Beverly Hills Periodontics & Dental Implant Center








Recent Comments